Ivermectin May Defeat Cancer and Other Common Chronic Diseases of Aging
If you think Big Pharma had good reasons to censor ivermectin during COVID-19 how about now when we know it is likely effective against all chronic diseases associated with aging?
Dr. Paul Marik recently quoted a prospective clinical trial where the participants were given 4000 international units of Vitamin D, omega 3’s and told to exercise and the risk of cancer dropped 50%.
In another post, Dr. Marik says it is highly unlikely cancer is genetically determined.
I wanted to talk about both in this post.
In July 1994, I published a new theory of cancer in Molecular Carcinogenesis which implied while tumors were genetically determined, the malignant nature of tumors (ie., the thing we call cancer) was not [1].
This notion that malignancy was a phenotype and not a genotype was heretical at the time and so the paper was ignored (only the editors of Molecular Carcinogenesis and myself were excited). It was an exciting idea because it meant one can control the malignant potential of tumors pharmacologically. No more need for slash and burn, which I have always regarded as barbaric.
However, subsequently it became widely accepted that the malignant phenotype of cancers called ‘epithelial mesenchymal transition’ (EMT) was real [2]. So I was vindicated, although it seems no one noticed except for myself.
The reason I had proposed cancer as a phenotype was that I had just finished the characterization of the 67 kD alpha-fetoprotein (AFP) receptor for my Ph.D. thesis [3-6]. The AFP receptor (AFPr) [4] was expressed on macrophages [3,6] and highly overexpressed on the common cancers the adenocarcinomas (breast, prostate, lung, colon, etc) [3,5] implying a dual role in immunosuppression of the host and in tumor malignant potential. In fact I wrote the theory to explain how immunosuppression of the host relates to tumor malignant potential.
AFP was the very first immunosuppressive factor described (1974) and the first tumor marker discovered (1963). We were first to show it prevented cell lysis (apoptosis) of macrophages in 1994 [6].
It is now well established that AFP contributes to the malignant phenotype through the PI3K/Akt/mTOR pathway, the same one conferred by malignancy-promoting HER-2/neu (ERBB2).
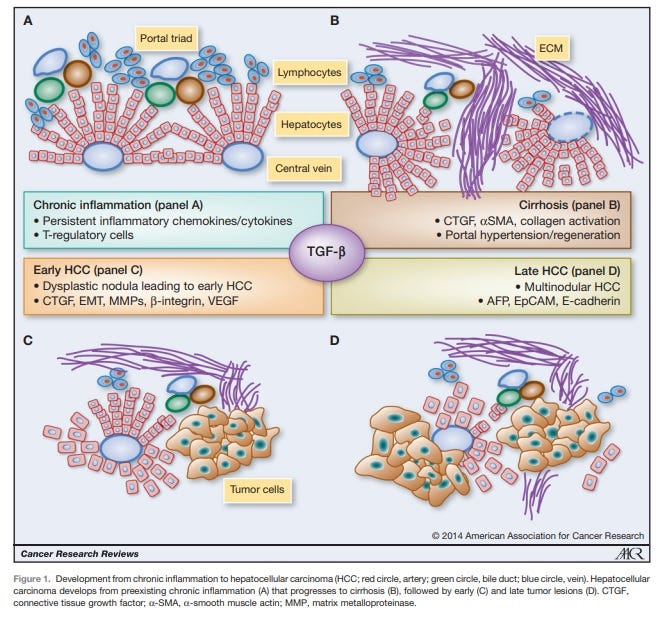
Figure 1. From Giannelli G et al, Cancer Research 2014 [7]. AFP is recognized as a malignancy progression factor in a very common cancer in the world, hepatocellular carcinoma (HCC) which is often associated with a viral origin.
Thus, the malignant potential of tumors known as cancer was amenable to pharmacological intervention and by entities that inactivate AFP.
AFP exists in active and inactive states. Things that bind to and inactivate AFP (zinc, DHEA, flavonoids etc) are entities that may help promote innate immunity (of macrophages) and which also diminish the malignant potential of tumors.
At the time I called this malignant phenotype of cancers “anti-cellular senescence” [1]. This was because the tumor was refractory to new signaling since AFP binding to the AFPr on tumors blocked incoming signals. So it seemed the tumor did not change or age because it couldn’t respond to cell signals. {Note anti-aging at the cellular level is associated with aging at the whole host level.}
While the malignant phenotype is now recognized as ‘epithelial-mesenchymal transition’ (EMT), fortunately Dr. Robert Weinberg has included the phenotype of blocking senescence as salient to EMT [8] ie., EMT is a phenotype involving anti-cellular senescence (whew!).
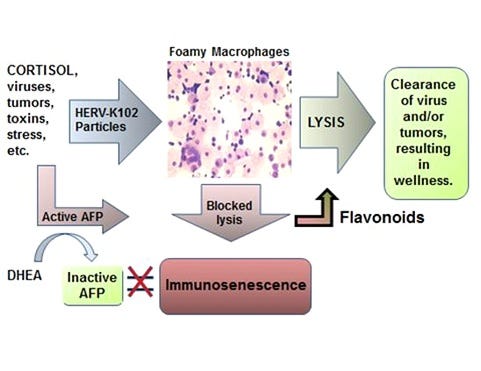
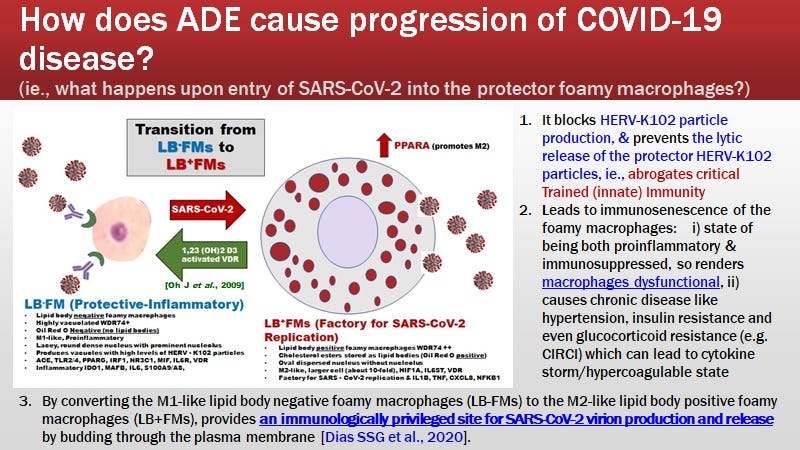
Then in 2015, I wrote the new immunosenescence paradigm of macrophages published in Discovery Medicine (Figure 2) which attempts to explain the cause of chronic illness associated with aging including diseases such as cancer and cardiovascular diseases [9].
Noteworthy, the immunosenescence of macrophages involves immunosuppression AND paradoxically the uncontrolled release of pro-inflammatory factors such as IL-6, TNF-alpha and IL-1beta. It is the inflammation that contributes to the start of chronic diseases. This would be exacerbated by ongoing infections due to the immunosuppression.
AFP by binding the 67 kD AFPr on foamy macrophages (M1-like), induces immunosuppression and prevents the down-modulation of the inflammatory factors. It is believed the inflammation is through activation of NFKB1 (see later). So immunosenescence of macrophages involves immune suppression and concomitant release of pro-inflammatory factors (the latter which cannot be down-regulated).
Figure 2. The New Immunosenescence Paradigm of Macrophages
was defined as the failed (lytic) release of protector HERV-K102 particles from foamy macrophages. HERV-K102 is a non-pathogenic, protector foamy retrovirus unique to humans which renders macrophages foamy (the particles accumulate in vacuoles in the cytoplasm giving the cells a foamy appearance). When the DHEA/cortisol ratio is low, there is a higher risk of immunosenescence upon exposures to virus due to inadequate levels of DHEA to bind and inactivate AFP. We reported in 1994 that AFP blocks apoptosis of macrophages [6]. Thus, the failed lytic release of the protector HERV-K102 particles is due to AFP. Therefore, AFP causes immunosenescence of macrophages.
Subsequently I validated this paradigm specifically for explaining the initiation and progression of cardiovascular diseases (CVD) [10]. Note that high cholesterol does not induce atherosclerosis or CVD. So it is a fallacy that lowering cholesterol such as by statins reduces cardiovascular risks. Statins do however prevent the activation of the macrophages to become foamy by blocking the cholesterol (mevalonate) pathway and which blocks CRITICAL trained (innate) immunity [11,12].
STATIN use is NOT a very wise choice (which blocks CRITICAL innate immunity) during pandemics or when fighting cancers, especially turbo cancers!
Stress and infections cause the activation of macrophages to become foamy. Indeed when the macrophages become foamy they express ACE (not ACE2) which increases blood pressure. After 7 days, when the foamy macrophages undergo apoptosis (cell lysis) to release the protector HERV-K102, the blood pressure goes back to normal (no more foamy macrophages expressing ACE so no more elevated blood pressure).
On the other hand, if the infection occurs when the DHEA/cortisol ratio is insufficient (such as in the unhealthy elderly or stressed), on day 7 the foamy macrophages fail to release the HERV-K102 particles and you have immunosenescence. Over time, the blood pressure will increase. This may be why hypertension is a very common risk factor for severe COVID-19 disease because it signifies your CRITICAL trained (innate) immunity is compromised.
As shown in Figure 2 the vacuoles and high levels of HERV-K102 protector particles require high levels of cholesterol. So one really needs to preserve the cholesterol pathway during infections.
P53 along with TGF-beta, represses AFP expression [13], and p53 is a tumor suppressor commonly deleted or at least dysfunctional in tumors/cancers.
ZBTB20 is a zinc finger transcription factor credited with post-natal down-regulation of AFP. However, when functional p53 is absent, it upregulates AFP [14].
Did you know that ZBTB20 is required for the induction of NFKB1 [15] such as when SARS-CoV-2 infects foamy macrophages in vivo by antibody dependent enhancement of infection (ADE) [16] which contributes to cytokine storm? AFP is significantly upregulated by SARS-CoV-2 infection at the protein and mRNA level in cell lines [17].
Referring back to Figure 2, AFP antagonists reverse and prevent immunosenescence. Immunosenescence causes age-associated chronic diseases [9,10]. This means AFP antagonists like zinc, flavonoids, DHEA/7-ketoDHEA, Vitamin D3 over 60 ng/ml, and now also ivermectin [18] are likely AFP antagonists which are therefore, predicted to reduce the risks of age-associated chronic illness including cancer, cardiovascular disease, a higher risk of infections, etc..
There is now in addition to many reports on how ivermectin behaves as a potent antiviral, emerging evidence for its reversion of the malignant phenotype particularly by inducing apoptosis [19] and blocking metastasis [20]. In other words ivermectin which doesn’t make your hair fall out, should be able to render any malignant tumors benign because it addresses the cause of “cancer”. Barbaric radiation therapies and chemotherapy, bone marrow transplants and the like, are allegedly no longer required.
The same probably also goes for most chronic diseases associated with aging with the exception of central nervous system disorders (which are often not reversible).
So if you think the war on ivermectin is over, in fact, it is just getting STARTED.
REFERENCES
Laderoute MP. A new perspective on the nature of the cancer problem: anti-cellular senescence. Mol Carcinog. 1994 Jul;10(3):125-33. doi: 10.1002/mc.2940100303.
Zhang Y, Weinberg RA. Epithelial-to-mesenchymal transition in cancer: complexity and opportunities. Front Med. 2018 Aug;12(4):361-373. doi: 10.1007/s11684-018-0656-6.
Laderoute MP. The Characterization of a Novel, Widespread, PNA-Reactive Tumor Associated Antigen: the Alpha-fetoprotein Receptor/Binding Protein. Ph.D. Thesis. The University of Alberta. Canada 1991, pp 256. https://era.library.ualberta.ca/items/6f548eb6-49a2-456c-b472-41f68976077f.
Moro R, Tamaoki T, Wegmann TG, Longnecker BM, Laderoute M. Monoclonal antibodies directed against a widespread oncofetal antigen: the alpha-fetoprotein receptor. Tumor Biology 1993 14 (2):116-130. Https: //doi.org/10.1159/000217864.
Laderoute M, Willans D, Wegmann T, Longenecker M. The identification, isolation and characterization of a 67 kilodalton, PNA-reactive autoantigen commonly expressed in human adenocarcinomas. Anticancer Res. 1994 May-Jun;14(3B):1233-45.
Laderoute MP, Pilarski LM. The inhibition of apoptosis by alpha-fetoprotein (AFP) and the role of AFP receptors in anti-cellular senescence. Anticancer Res. 1994 Nov-Dec;14(6B):2429-38.
Giannelli G, Villa E, Lahn M. Transforming growth factor-β as a therapeutic target in hepatocellular carcinoma. Cancer Res. 2014 Apr 1;74(7):1890-4. doi: 10.1158/0008-5472.CAN-14-0243.
Weinberg RA. Twisted epithelial-mesenchymal transition blocks senescence. Nat Cell Biol. 2008 Sep;10(9):1021-3. doi: 10.1038/ncb0908-1021.
Laderoute MP. A new paradigm about HERV-K102 particle production and blocked release to explain cortisol mediated immunosenescence and age-associated risk of chronic disease. Discov Med. 2015 Dec;20(112):379-91.
Laderoute M. The paradigm of immunosenescence in atherosclerosis-cardiovascular disease (ASCVD). Discov Med. 2020 Jan-Feb;29(156):41-51.
Bekkering S, Arts RJW, Novakovic B, et al. Metabolic induction of trained immunity through the mevalonate pathway. Cell. 2018 Jan 11;172(1-2):135-146.e9. doi: 10.1016/j.cell.2017.11.025.
Bekkering S, Quintin J, Joosten LA, van der Meer JW, Netea MG, Riksen NP. Oxidized low-density lipoprotein induces long-term proinflammatory cytokine production and foam cell formation via epigenetic reprogramming of monocytes. Arterioscler Thromb Vasc Biol. 2014 Aug;34(8):1731-8. doi:
Wilkinson DS, Ogden SK, Stratton SA, Piechan JL, Nguyen TT, Smulian GA, Barton MC. A direct intersection between p53 and transforming growth factor beta pathways targets chromatin modification and transcription repression of the alpha-fetoprotein gene. Mol Cell Biol. 2005 Feb;25(3):1200-12. doi: 10.1128/MCB.25.3.1200-1212.2005.
To JC, Chiu AP, Tschida BR, Lo LH, Chiu CH, Li XX, Kuka TP, Linden MA, Amin K, Chan WC, Bell JB, Moriarity BS, Largaespada DA, Keng VW. ZBTB20 regulates WNT/CTNNB1 signalling pathway by suppressing PPARG during hepatocellular carcinoma tumourigenesis. JHEP Rep. 2020 Dec 19;3(2):100223. doi: 10.1016/j.jhepr.2020.100223.
Liu X, Zhang P, Bao Y, Han Y, Wang Y, Zhang Q, Zhan Z, Meng J, Li Y, Li N, Zhang WJ, Cao X. Zinc finger protein ZBTB20 promotes Toll-like receptor-triggered innate immune responses by repressing IκBα gene transcription. Proc Natl Acad Sci U S A. 2013 Jul 2;110(27):11097-102. doi: 10.1073/pnas.1301257110.
Ren X, Wen W, Fan X, et al. COVID-19 immune features revealed by a large-scale single-cell transcriptome atlas. Cell. 2021 Apr 1;184(7):1895-1913.e19. doi: 10.1016/j.cell.2021.01.053.
Appelberg S, Gupta S, Svensson Akusjärvi S, et al. Dysregulation in Akt/mTOR/HIF-1 signaling identified by proteo-transcriptomics of SARS-CoV-2 infected cells. Emerg Microbes Infect. 2020 Dec;9(1):1748-1760. doi: 10.1080/22221751.2020.1799723. (& personal communication).
Laderoute M. Ivermectin may prevent and reverse immunosenescence by antagonizing alpha-fetoprotein and downmodulating PI3K/Akt/mTOR hyperactivity. Open Heart. April 29, 2021. https://openheart.bmj.com/content/8/1/e001655.responses#ivermectin-may-prevent-and-reverse-immunosenescence-by-antagonizing-alpha-fetoprotein-and-downmodulating-pi3k-akt-mtor-hyperactivity.
Tang M, Hu X, Wang Y, Yao X, Zhang W, Yu C, Cheng F, Li J, Fang Q. Ivermectin, a potential anticancer drug derived from an antiparasitic drug. Pharmacol Res. 2021 Jan;163:105207. doi: 10.1016/j.phrs.2020.105207.
Jiang L, Sun YJ, Song XH, Sun YY, Yang WY, Li J, Wu YJ. Ivermectin inhibits tumor metastasis by regulating the Wnt/β-catenin/integrin β1/FAK signaling pathway. Am J Cancer Res. 2022 Oct 15;12(10):4502-4519.



The issue of turbo cancers after exposures to spike protein is a very real concern. Most likely ivermectin will help greatly... sooner better than later.
I'm curious if IVM or Fenben help mitigate Malaria, You know because Bill Gates and all those evil scientists have released mosquitos that carry malaria and now there is a small outbreak in Florida and Texas. I see that Intravenous quinidine gluconate in the treatment of severe Plasmodium falciparum but wondered if IVM or Fenben could be appropriate?